Spinal disc replacement surgery has emerged as a motion-preserving alternative to spinal fusion, offering significant relief for patients with degenerative disc disease. Dr. Larry Davidson, an experienced surgeon in the field, recognizes that while the procedure’s success depends on surgical precision and the quality of the implant, an often-overlooked factor is the role of spinal biomechanics. Understanding how forces, alignment and movement patterns within the spine influence surgical outcomes is essential for achieving long-term success.
The Basics of Spinal Biomechanics
Spinal biomechanics refers to the study of how the spine moves and handles forces during daily activities. The spine is a highly dynamic structure composed of vertebrae, discs and ligaments that work together to support the body and allow movement. Each spinal segment is intricately linked, and changes in one area can affect the biomechanics of the entire spine.
Key elements of spinal biomechanics include load distribution, range of motion and alignment. These factors play a critical role in determining the spine’s functionality and response to interventions like disc replacement. Proper load distribution ensures even stress across spinal segments, reducing the risk of adjacent segment degeneration. Similarly, maintaining alignment and natural motion is essential for optimal implant performance and long-term spinal health.
The Role of Biomechanics in Disc Replacement Surgery
Load Distribution
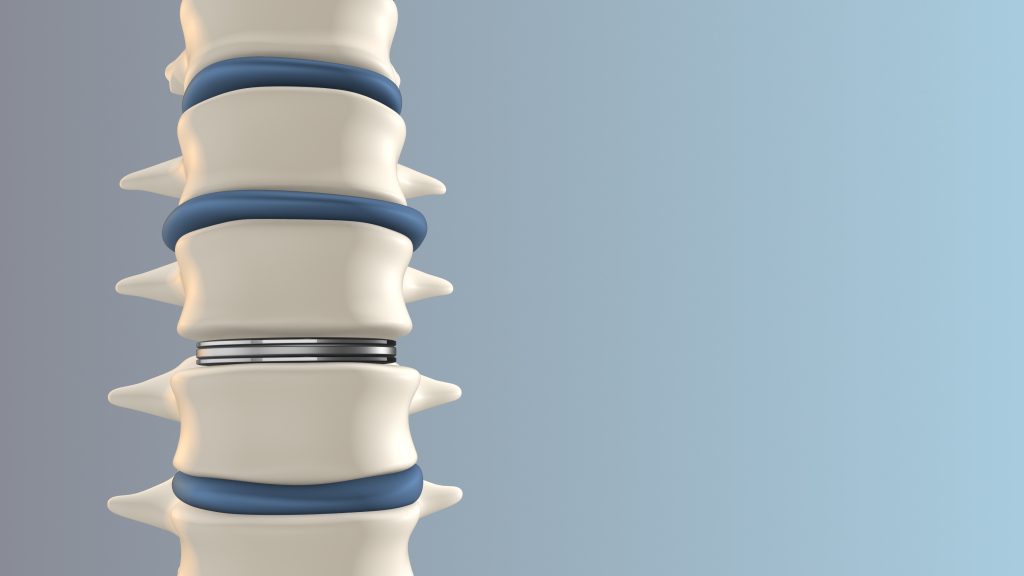
One of the primary goals of disc replacement surgery is to restore normal load distribution within the spine. A damaged or degenerated disc often causes uneven weight-bearing, leading to strain on adjacent discs and joints. An artificial disc mimics the function of a natural disc, helping to evenly distribute forces across the spine. Proper load distribution reduces the risk of complications like adjacent segment degeneration and improves the durability of the implant.
Range of Motion
Artificial discs are designed to preserve the natural range of motion at the treated spinal level. This motion preservation is a key advantage of disc replacement over spinal fusion, which eliminates movement at the fused segment. By maintaining flexibility, the spine can move more naturally, reducing stress on adjacent levels and enhancing overall functionality.
Spinal Alignment
Correct spinal alignment is crucial for the success of disc replacement surgery. Misalignment, such as kyphosis or lordosis, can alter the spine’s biomechanics, leading to uneven implant wear and increased stress on surrounding tissues. Precise placement of the artificial disc ensures proper alignment, promoting optimal biomechanics and reducing the risk of implant failure.
How Biomechanical Factors Affect Surgical Outcomes
Implant Performance
The success of an artificial disc depends largely on how well it integrates with the surrounding spinal structures. Proper biomechanics ensure that the implant functions as intended, preserving motion and maintaining stability. Poor alignment or incorrect sizing of the implant can disrupt biomechanics, leading to pain, limited mobility or the need for revision surgery.
Adjacent Segment Protection
One key benefit of disc replacement is its ability to protect adjacent segments from degeneration. By preserving motion and distributing forces evenly, the procedure minimizes the stress placed on neighboring discs. However, if spinal biomechanics are not properly addressed, adjacent segments may still experience excessive strain, negating this benefit.
Patient-Specific Considerations
Every patient’s spinal biomechanics are unique and influenced by factors such as posture, activity level and overall spinal health. Tailoring the procedure to the patient’s specific biomechanics improves outcomes. For instance, a patient with a sedentary lifestyle may have different biomechanical needs than an active individual engaging in high-impact activities.
The Importance of Preoperative Planning
Comprehensive preoperative planning is essential to address biomechanical factors and ensure the success of disc replacement surgery. Advanced imaging techniques, such as MRI and CT scans, provide detailed insights into the patient’s spinal alignment, disc health and load distribution. Surgeons use this information to determine the optimal size, position and type of artificial disc for each patient.
Biomechanical simulations are also becoming an integral part of preoperative planning. These simulations predict how the spine will respond to the implant, allowing surgeons to make data-driven decisions that improve outcomes.
Innovations Enhancing Biomechanical Precision
Recent advancements in technology are helping surgeons optimize spinal biomechanics during disc replacement surgery. Robotic-assisted surgery allows for greater precision in implant placement, ensuring proper alignment and load distribution. 3D-printed implants tailored to the patient’s anatomy further enhance biomechanical compatibility.
Additionally, the integration of motion sensors and real-time imaging during surgery provides immediate feedback, allowing surgeons to make adjustments that align with the patient’s natural biomechanics. These innovations not only improve surgical accuracy but also reduce the risk of complications.
Long-Term Implications of Spinal Biomechanics
Spinal biomechanics have a lasting impact on the success of disc replacement surgery. Properly restored biomechanics reduce the likelihood of adjacent segment degeneration, implant failure and chronic pain. Patients benefit from improved mobility, reduced discomfort and a higher quality of life.
Dr. Larry Davidson emphasizes, “Emerging minimally spinal surgical techniques have certainly changed the way that we are able to perform various types of spinal fusions. All of these innovations are aimed at allowing for an improved patient outcome and overall experience.” These advancements not only enhance surgical precision but also reduce recovery times, making spinal procedures more accessible and effective for a wider range of patients.
However, achieving these outcomes requires ongoing attention to spinal health. Regular follow-ups, physical therapy and maintaining a healthy lifestyle are crucial for preserving the biomechanics established during surgery.
Spinal biomechanics are a fundamental factor in the success of disc replacement surgery, influencing everything from implant performance to long-term outcomes. By restoring proper load distribution, range of motion and alignment, the procedure enhances functionality and reduces the risk of complications. Advances in preoperative planning, surgical technology and implant design are further refining the ability to optimize spinal biomechanics, ensuring better results for patients.
Understanding the importance of biomechanics underscores the need for a tailored approach and an experienced surgical team for those considering spinal disc replacement. With the right planning and execution, patients can achieve lasting pain relief and restored mobility, transforming their quality of life.